Preparing Health Systems for integrated and personalized care
At the recently concluded DIA Europe 2020, Roche hosted a session that focused on this very topic called "Preparing Health Systems for integrated and personalised care". How can policymakers, healthcare providers and patients move on from the one-size-fits-all treatment focus of today?
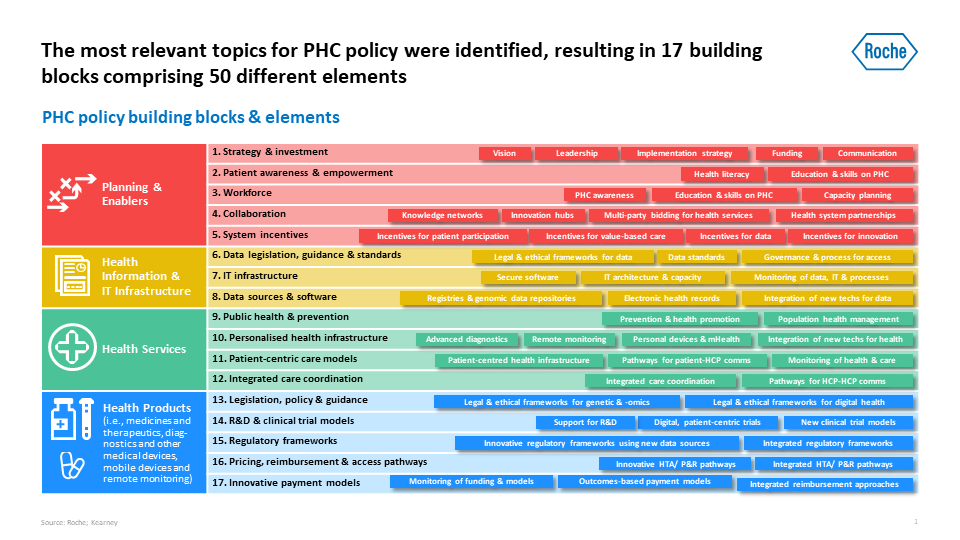
In 2020 Roche launched a multi-stakeholder project to identify the building blocks that underpin personalised healthcare and review how they are addressed in countries’ health plans. The building blocks are the underlying units of any health system, which are critical to support personalised healthcare. More than 80 plans from 20 countries were screened and 15 analysed in detail in order to identify the critical building blocks of a holistic and integrated personalised healthcare system plan. These were then validated through a number of expert interviews and a full-day roundtable with leading experts in precision health and genomics, digital health, public health and health strategy.
On June 30th, we were happy to welcome leading health voices Nick Guldemond (Leiden University Medical Centre), Pierre Meulien (IMI, Executive Director), Michelle Rohrer (Senior Vice President, Global Head of Product Development Regulatory & Policy at Hoffmann La Roche) and Usman Khan (Managing Director Modus Europe, former Executive Director European Patients’ Forum) to a thoroughly engaging panel discussion on how we can take the Building Blocks framework and begin building personalised healthcare, together.
The conversation was guided by Tom Brookland, a Personalised Healthcare Policy Strategy Lead at Roche.
Regulatory challenges
Regulatory frameworks can play a key role when it comes to supporting the uptake of personalised health. In order to shift towards health systems that are fully integrated and personalised, regulatory frameworks should be updated to enable the use of diverse types of information, such as real-world evidence and digital endpoints, to complement clinical trials and provide an iterative view of health products’ safety and efficacy. Additionally, we should ensure that regulatory frameworks are integrated, so that they can go beyond the traditional assessment of a medicine, and evaluate combinations of medicines, diagnostics and digital technologies, tailored to the individual patients.
As Michelle Rohrer points out, healthcare innovations are greatly diminished without such an integrative approach: “If we think about how it feels to be a patient today, even with innovative solutions such as digital, big data, CDS tools etc., if you are diagnosed with a disease it still feels like you are lost in space and on your own. Despite great healthcare providers out there who are trying their best – everything still works in isolation of each other and hence it is very lonely as a patient. It is time we as providers begin to really think in this integrated solution perspective”.
Patient perspectives and priorities
Usman Khan stated that; "Our healthcare is fundamentally population-based and paternalistic, and we need to move towards a position where it is individual and patient centred. Moving towards personalised health is important because that is going to be the only way that we can really achieve patient-centred care."
Personalised healthcare can become a reality only with the support of a wide range of engaged stakeholders. In this context, it is crucial that citizens and patients are empowered to understand the potential of personalised healthcare in health management from prevention to end of life.
Education for citizens and patients on topics such as digital, data and personalised healthcare can help to ensure they are comfortable using digital health, sharing their data and providing consent accordingly, or understanding the risks and benefits of different choices in healthcare.
Public private partnerships
The COVID-19 crisis is showing that public-private partnerships are needed for delivering on the needs of healthcare systems, citizens and patients. The shift towards personalised health makes no difference: it can only be achieved with stronger ties between public and private stakeholders, and through public support for R&D, which should co-fund continued innovation and, eventually, translation of research findings into clinical practice. At the same time, stronger collaboration across geographies between governments, patients, HCPs, academia, and innovators is needed to bridge gaps in funding and skills from either side and scale up accessible innovation.
Such public-private partnerships can result in broad coalitions. Pierre Meulien explains: “Many IMI projects link to the concept of personalised medicine, attempting to decipher the taxonomy of diseases, and one project that comes to mind is “U-BIOPRED”, a project in severe asthma trying to dissect asthma into subtypes of severe asthma. This is a typical kind of IMI project, one of the first ones launched in 2009, which involved 12 companies, universities, and importantly 5 patient groups involved who took a key role.”
Our thanks to DIA Europe for hosting this important event.
To read more about these topics, please take a look at our Consensus Paper, which summarizes and condenses all the research we have put into understanding the next evolution of our health systems.
Let's build personalised healthcare, together.
Read the full consensus paper here.