2. How can technology speed up system-level changes and improve health delivery?
Data shows Quality and Access are two priority areas that need to be approached holistically by policymakers in order to make an impact in achieving Universal Health Coverage (UHC). For example, many Africans do not receive preventative treatment for reasons outside of their control, predominantly due to distance from healthcare facilities, or a lack of resources. This reality is reflected in the Index results showing that countries with relatively good access to services do not necessarily come first on the quality of the health services provided, and vice-versa. On the one hand, South Africa and Morocco make it in the top 5 on both quality and access, and also top the overall Index, showing a positive correlation between good access to, quality of health services and the sustainability of a healthcare system. On the other hand, a country like Tanzania has high quality health services, but limited access, while Libya scores well on access but could improve on quality.

Seth Akumani of the United Nations Development Program in Ghana believes that, beyond developing appropriate policy solutions, a key remedy to national challenges will be putting technology at the heart of developing sustainable healthcare solutions. Taking advantage of Africa’s massive and still growing mobile accessibility could bring healthcare to people directly. There are already significant mobile initiatives that provide both medical advice and health awareness campaigns to millions of Africans, such as “Be He@lthy, Be Mobile” (BHBM) set up by the WHO and International Telecommunications Union (ITU), and Vodafone's “Mum & Baby” program for expectant parents in South Africa. Limited infrastructure can also be circumvented through the clever use of digital solutions, such as the recent deliveries of COVID-19 tests across Ghana using drones.
Survey results
Actions to be taken
Amidst the global transition towards digital technologies certain regions are left behind due to a lack of necessary infrastructure, capabilities and resources, thereby creating a digital divide. Digitisation in the health sector is deemed vital in transforming African healthcare to create a sturdy health ecosystem grounded in technology. With a large youth population, the continent is well placed to take advantage of innovative technology in facilitating wider access and quality of healthcare that boosts the quality of life of African citizens.
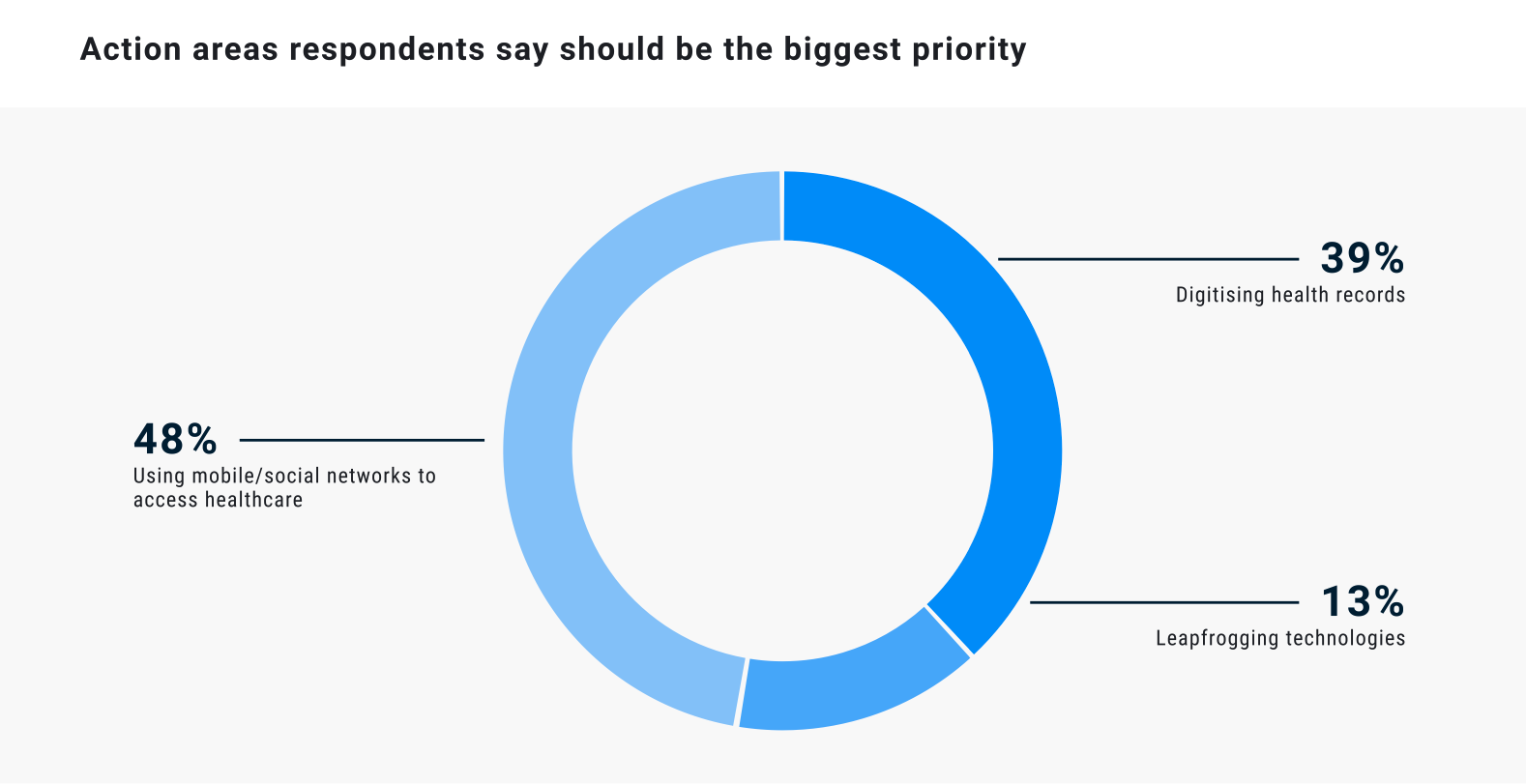
Mobile healthcare will allow broadscale access to a majority of the population, something aided by Africa’s young population who are major consumers in the mobile phone market now and for the foreseeable future. This is evident from our survey, where almost half (48%) agreed that using mobile/ social networks to access healthcare should be the biggest priority for the health sector.
Geographical inequalities in Africa are stark. These often translate to inequality in access to health services. Digitalising health services can be of tremendous help to serve patients who live in hard to reach areas.

Organisations that will have the biggest impact
The private sector plays an increasingly large role in boosting technological innovations that enable system-level change in healthcare across Africa. The largest portion of respondents (39%) identified using mobile/social networks to access healthcare as the area where public sector focus can make the biggest difference

Policy Recommendations
How can technology speed up system-level changes and improve health delivery?
- Make the implementation of strategic innovation policies, sound infrastructure and strong technology standard-setting institutions an absolute priority.
- Allow mHealth to become a driver for change. Since it is focused on the citizen, mHealth empowers patients to manage their own health and wellbeing. Realising the potential of this innovation requires clear leadership and supportive policies.
- Restructure financial models from those which reward work being completed to those incentivising outcomes achieved. mHealth reduces costs and enables better patient outcomes, so reimbursement should reward the switch to this model and encourage uptake, e.g., through more online consultations.
- Appoint a regional- and national- level coordinator for eHealth and publish an action plan which includes the use of telemedicine.
- Introduce new legislation in the countries where e-health is still not the norm, to remove barriers to online health consultations.
- Improve the policy and regulatory landscape supporting closed end-to-end transactions. In the short term such improvements can focus on improving clarity of mHealth regulations.

Case Study
Using mobile/ social networks to access healthcare
- M-Pesa example, Kenya and Tanzania
- Make the implementation of strategic innovation policies, sound infrastructure and strong technology standard-setting institutions an absolute priority.
- Allow mHealth to become a driver for change. Since it is focused on the citizen, mHealth empowers patients to manage their own health and wellbeing. Realising the potential of this innovation requires clear leadership and supportive policies.
- Restructure financial models from those which reward work being completed to those incentivising outcomes achieved. mHealth reduces costs and enables better patient outcomes, so reimbursement should reward the switch to this model and encourage uptake, e.g., through more online consultations.
- Appoint a regional- and national- level coordinator for eHealth and publish an action plan which includes the use of telemedicine.
- Introduce new legislation in the countries where e-health is still not the norm, to remove barriers to online health consultations.
- Improve the policy and regulatory landscape supporting closed end-to-end transactions. In the short term such improvements can focus on improving clarity of mHealth regulations.